
Eloise’s at-home oxygen concentrator
Eloise’s condition has been around long enough and isn’t going anywhere, so I feel like now is a good time to explain her diagnosis and what’s happened these past four months. I’ve kept most of her health concerns quiet and off social media for the longest time because we didn’t, and still don’t, have all the answers that we’re looking for; there were/are more questions than answers. And to be honest, “I don’t know,” were the autoresponses to a lot of questions we received from close friends and family, and it started taking a toll on us emotionally. While we don’t know a whole lot about her condition, we do have some information that will hopefully explain what’s going on.

Eloise at four months old.
Eloise has been diagnosed with central apnea, a condition in which her body decreases and stops its effort to breathe. This is unobstructive, meaning she doesn’t have any physical reason for her lack of breathing, like enlarged tonsils, etc. Central apnea is often related to an underdeveloped brain stem, so we don’t have a real timeline as to when she’ll grow out of this condition; it’s all up to her body and her development. What we’ve been told and have read online is that central apnea babies are usually pre-term, and most outgrow it by their 44th gestational week equivalent. What makes Eloise’s condition fairly unique is that she was delivered full-term at 38 weeks and still continues to suffer from apnea episodes, even at four months old. What makes apnea so scary is that the long periods of lack of oxygen decreases the level of oxygen in the blood and increases the amount of carbon dioxide in her body, can cause bradycardia (heart rate plummet to less than 60 beats per minute) which makes self-recovery from an apnea episode even harder, can lose consciousness, and can cause brain damage if the apnea episode persists for longer than 45 seconds.

Our first family photo on August 3rd, the first time Eloise had been released from observation for a quick family photo.
When Eloise was born, her delivery was uneventful but she did stop breathing three times within the first 14 hours of her life. Instead of being placed in the NICU, she stayed in the hospital for an extra day under close observation and was then sent home. Five nights later on August 9th, at eight days old, I found her in her bassinet not breathing and had to resuscitate her before rushing to the pediatric ER. She stayed in PICU for three days after lots of testing, and was released with an apnea monitor to be worn 24/7.

Eloise in observation at the hospital at two days old.

This photo was taken just hours before I found her unresponsive in her bassinet at eight days old.

Eloise in the PICU at nine days old.
We followed up with a pediatric pulmonologist for more testing, and had two sleep studies performed. The first sleep study (done at 13 days old) showed that she would stop breathing for longer than 17 seconds on average of 28 times per hour. The very next night we had another sleep study performed, this time with oxygen therapy delivered with a nasal cannula, but she had an adverse response to the oxygen and stopped breathing on average of 40 times per hour lasting longer than 17 seconds. This threw us back into the hospital for an entire week in the PICU again with lots of tests that confirmed her central apnea diagnosis.
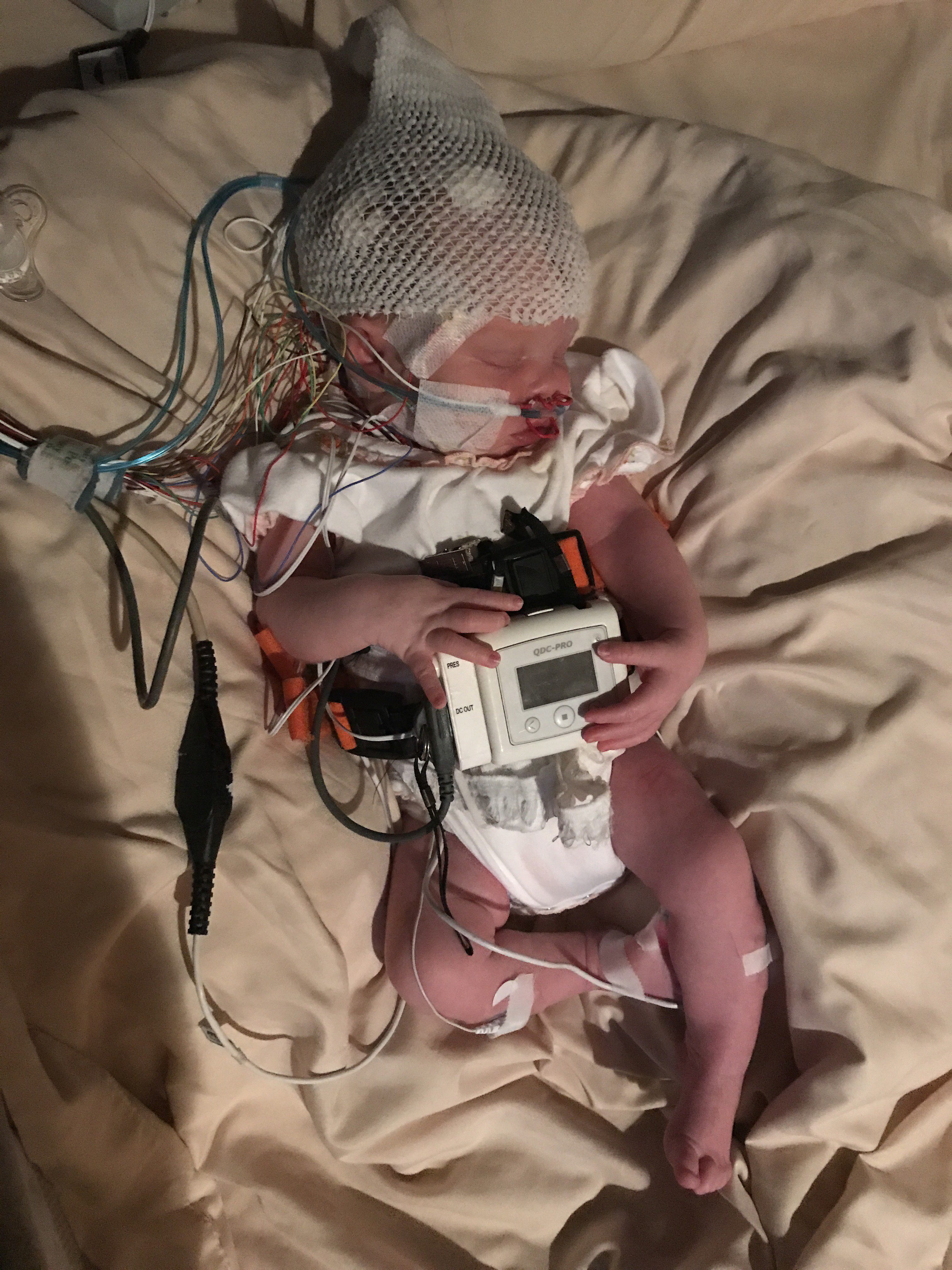
Eloise in her second sleep study at two weeks old.

Eloise in the hospital in the PICU for a week in August and September.
Eloise has been on, and still is, on medication called caffeine citrate that is used to stimulate her nervous system to “remind” her to breathe, as well as reflux medications to combat the caffeine citrate’s side-effects. She’s still on the apnea monitor and will be for at least six more months, and had her oxygen concentrator and oxygen tanks delivered yesterday.

To be completely honest, I haven’t given E’s condition much thought; I do think about it when I need to, but most of the time I see a smiling, giggly baby who looks completely healthy. I’m still in survival mode, all while trying to keep Walter’s normal routine, well, normal because I don’t want him to think that something is wrong with Eloise. Do I hide everything about E’s condition away from him? No, but I try to keep the “special treatment” of her at a minimum in front of W. An oxygen tank and an apnea monitor won’t keep us away from doing the things we love, like Disney, but it does take a heavy spoonful of patience. It’s just a season, and we’ll get through this.


